Vaccines that protect against Covid-19 are on the way. What should older adults expect?
The first candidates, from Pfizer and Moderna, could arrive by the end of this month, according to Alex Azar, who heads the Department of Health and Human Services.
Both vaccines are notably effective in preventing illness due to the coronavirus, according to information released by the companies, although much of the data from clinical trials is still to come. Both have been tested in adults age 65 and older, who mounted a strong immune response.
Seniors in nursing homes and assisted living centres will be among the first Americans vaccinated, following recommendations last week by a federal advisory panel. Older adults living at home will need to wait a while longer.
Many uncertainties remain. Among them: What side effects can older adults anticipate and how often will these occur? Will the vaccines offer meaningful protection to seniors who are frail or have multiple chronic illnesses?
Here’s a look at what’s known, what’s not and what lies ahead.
Decision-making timetable. Pfizer’s vaccine will be evaluated by a 15-member Food and Drug Administration advisory panel on Thursday. Moderna’s vaccine is expected to go before the panel Dec. 17.
At least two days before each meeting, an analysis by FDA staff will be made public. This will be the first opportunity to see extensive data about the vaccines’ performance in large phase 3 clinical trials, including more details about their impact on older adults.
So far, summary results disclosed in news releases indicate that Pfizer’s vaccine, produced in partnership with BioNTech, has an overall efficacy rate of 95% and efficacy of 94% in people 65 and older. Moderna’s overall efficacy is 94%, with 87% efficacy in preventing moderate disease in older adults, according to Moncef Slaoui, chief science adviser to Operation Warp Speed, the government’s Covid-19 vaccine development programme.
If the advisory panel gives a green light, the FDA will decide within days or weeks whether to authorise the Pfizer and Moderna vaccines for emergency use. Distribution of the vaccine has already begun, and health care providers are expected to begin administering it immediately after the FDA acts.
Allocation framework. At a Dec. 1 meeting of the Advisory Commission on Immunisation Practices (ACIP), which guides the Centers for Disease Control and Prevention on vaccines, experts recommended that people living in long-term care (primarily nursing homes and assisted living facilities) and healthcare workers be the first groups to get Covid-19 vaccines.
This recognises the extraordinary burden of Covid-19 in long-term care facilities. Although their residents represent fewer than 1% of the US population, they account for 40% of Covid deaths – more than 100,000 deaths to date.
The commission’s decision comes despite a lack of evidence that Pfizer’s and Moderna’s vaccines are effective and safe for frail, vulnerable seniors in long-term care. Vaccines were not tested in this population. Federal officials insist side effects will be carefully monitored.
Next in line likely would be essential workers who cannot work from home, such as police, firefighters, teachers and people employed in food processing and transportation, according to commission deliberations Nov. 23 that have not come to a formal vote.
Then would be adults with high-risk medical conditions such as diabetes, cancer, kidney disease, obesity, heart disease and autoimmune diseases and all adults age 65 and older.
Although states typically follow ACIP guidelines, some states may choose, for instance, to vaccinate high-risk older adults before some categories of essential workers.
Left off the list are family caregivers, who provide essential support to vulnerable older adults living in the community – an unpaid workforce of tens of millions of people. “If someone is providing day-to-day care, it makes sense they should have access to the vaccine, too, to keep everyone safe,” said Beth Kallmyer, vice president of care and support for the Alzheimer’s Association.
Further prioritisation. The priority groups constitute nearly half of the US population – 21mn healthcare workers, 3mn long-term care residents, 66mn essential workers, more than 100mn adults with high-risk conditions and 53mn adults age 65 and older.
With initial supplies of vaccines limited, setting priorities will be inevitable. Practically, this means that hospitals and physicians may try to identify older adults who are at the highest risk of becoming seriously ill from Covid-19 and offer them vaccines before other seniors.
A study of more than 500,000 Medicare beneficiaries age 65 and older provides new evidence that could influence these assessments. It found the conditions that most increase older adults’ chances of dying from Covid-19 are sickle cell disease, chronic kidney disease, leukaemias and lymphomas, heart failure, diabetes, cerebral palsy, obesity, lung cancer and heart attacks, in that order.
“Out of all Medicare beneficiaries, we identified just under 2,500 who had no medical problems and died of Covid-19,” said Dr Martin Makary, co-author of the study and a professor of health policy and management at Johns Hopkins Bloomberg School of Public Health in Baltimore. “We knew risk was skewed toward comorbidity [multiple underlying medical conditions], but we didn’t realise it skewed this much.”
Supplies available. Both the Pfizer and Moderna vaccines require two doses, administered three to four weeks apart. The companies have said about 40mn doses of their vaccines should be available this year, enough to fully vaccinate about 20mn people.
After that, 50mn doses might become available in January, followed by 60mn doses in both February and March, according to Dr Larry Corey, a virologist who heads the Covid-19 Prevention Trials Network.
That translates into enough vaccine for another 85mn people and should be sufficient to vaccinate older adults in addition to medical personnel on the front lines and many other at-risk individuals, Corey suggested at a recent panel on Covid-19 sponsored by the National Academy of Medicine and American Public Health Association.
He acknowledged these were estimates, based on information he has been given. Pfizer and Moderna have not yet specified how much vaccine will be delivered and when. Nor is it clear when other vaccines under investigation will become available – 13 are in phase 3 clinical trials – or what their monthly production capacity might be.
Distribution issues. As Pfizer’s and Moderna’s vaccines are rolled out, a very vulnerable group may have difficulty getting them: 2mn seniors who are homebound and another 5.3mn with physical impairments who have problems getting around.
The reason: handling and cold storage requirements.
Pfizer’s vaccine needs to be stored at minus 70C, calling for special equipment not available in small hospitals, clinics or doctors’ offices. Moderna’s vaccine needs long-term storage at minus 20C.
Landmark Health provides in-home medical care to more than 120,000 frail, chronically ill homebound seniors in 15 states. “We don’t have the capabilities to store and distribute these vaccines to our population,” said Dr Michael Le, the company’s co-founder and chief medical officer.
Instead, he said, Landmark is working to arrange transportation for its patients to centres where Covid-19 vaccines will be administered and educating them about the benefits of the vaccines. “Given the trust, the bond we have with our patients, we can play a big role as advocates,” Le said.
Addressing mistrust. Advocates have a big job ahead of them. According to a recent poll from the University of Michigan, only 58% of older adults (ages 50 to 80) said they were very or somewhat likely to get a Covid-19 vaccine. A significant number of older adults, 46%, thought they’d get the vaccine eventually but wanted others to go first. Only 20% wanted to get it as soon as possible.
Most important in making decisions is knowing how well the vaccine works, according to 80% of the 1,556 older adults surveyed. Just over half (52%) said a recommendation from their doctor would be influential.
Dr Sharon Inouye, a geriatrician at Hebrew Senior Life in Boston and a professor of medicine at Harvard Medical School, is among the physicians impatiently awaiting the publication of data from Pfizer’s and Moderna’s phase 3 clinical trials.
Among the things she wants to know: How many older adults with chronic health conditions participated? How many participants were 75 and older? Did side effects differ for older adults?
“What I worry about most is the side effects,” she said. “We may not be able to know about serious but rare side effects until millions of people take them.”
But that’s a gamble she’s willing to take. Not only will Inouye get a vaccine, she just told her 91-year-old mother, who lives in assisted living, to say “yes” when one is offered.
“My whole family lives in fear that something will happen to her every day,” Inouye said. “Even though there’s a lot we still don’t know about these vaccines, it’s compelling that we protect people from this overwhelming illness.
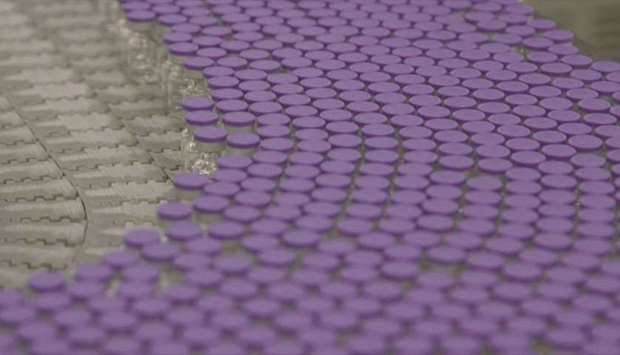
Images of the coronavirus vaccine being developed by US pharmaceutical giant Pfizer in Kalamazoo, Michigan, after the company announced its vaccine is u201c90% effectiveu201d against Covid-19 infections.
