There are currently over 199 million women living with diabetes and this total is projected to increase to 313 million by 2040. Diabetes is the ninth leading cause of death in women globally, causing 2.1 million deaths each year, says International Diabetes Federation, the non-profit association promoting diabetes care, prevention and cure worldwide.
As a result of socioeconomic conditions, girls and women with diabetes experience barriers in accessing cost-effective diabetes prevention, early detection, diagnosis, treatment and care, particularly in developing countries.
Diabetes and Pregnancy
We know that the key to a healthy pregnancy for a woman with diabetes is keeping blood glucose (sugar) in the target range – both before the patient gets pregnant and during her pregnancy. To do this, the patient needs a diabetes treatment plan that keeps meals, exercise and insulin in balance. This plan will change as they change with pregnancy. Patients will need to check their blood glucose often and keep a record of the results. With blood glucose in the target range and good medical care, the chances of a trouble-free pregnancy and a healthy baby are almost as good as they are for a woman without diabetes.
Before pregnancy: Despite advances, babies born to women with diabetes, especially women with poor diabetes control are still at greater risk for birth defects. For this reason, good blood glucose control before the patient gets pregnant is very important. If the blood glucose levels are not in good control, they need to be brought under control before pregnancy.
During pregnancy: Pregnancy is often a time of great highs and lows of blood sugar, so good prenatal care are essential. Many changes occur in the body due to the pregnancy and because of diabetes these changes will affect the blood glucose level. Pregnancy can also make symptoms of low blood glucose hard to detect. During pregnancy, diabetes control will require more work. The blood glucose checks the patients does at home are a key part of taking good care of herself and her baby before, during and after pregnancy.
What is gestational diabetes?
Pregnant woman who have never had diabetes before but who have high blood sugar (glucose) levels during pregnancy are said to have gestational diabetes. Gestational diabetes affects about 4% of all pregnant women. Gestational diabetes starts where the patient’s body is not able to make or use the insulin it needs. Without enough insulin, sugar (glucose) cannot leave the blood and be changed to energy. When sugar builds up in the blood to high levels, this is called High Blood Sugar (hyperglycaemia).
How to gestational diabetes can affect your baby?
Although insulin does not cross the placenta to the baby, sugar and other nutrients do. Since the baby is getting more sugar than it needs to grow and develop, the extra energy is stored as fat.
This can lead to a “fat” baby. Babies who are large at birth face health problems of their own, including damage to their shoulders during birth. Because of the extra insulin, newborns may have very low blood sugars at birth and are also at higher risk for breathing problems. Babies with excess insulin become children who are at risk for obesity and adults who are risk for serious type2 diabetes.
Gestational diabetes affects the mother in late pregnancy, after the baby’s body has been formed, but while the baby is busy growing. Because of this, gestational diabetes does not cause the kinds of birth defects sometimes seen in babies whose mothers had diabetes before pregnancy.
Treating gestational diabetes
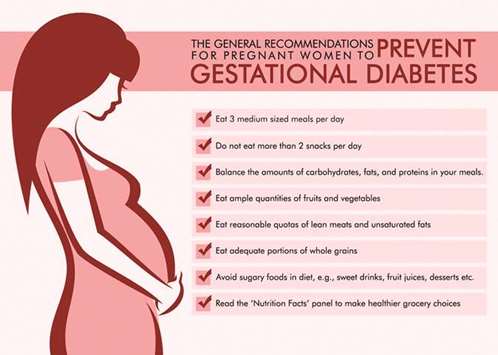
A treatment for gestational diabetes aims to keep blood glucose levels equal to those of pregnant women who don’t have gestational diabetes. A treatment for gestational diabetes always includes special meal plans and scheduled physical activity. It may also include daily blood sugar testing and insulin injections.
Insulin is the traditional first-choice drug for blood glucose control during pregnancy, because it is the most effective for fine-tuning blood glucose and it doesn’t cross the placenta. Therefore, it is safe for the baby. Insulin can be injected with a syringe, an insulin pen, or through an insulin pump. All three methods are safe for pregnant women.
Gestational diabetes – looking ahead
Gestational diabetes usually goes away after pregnancy. But once the patient has had gestational diabetes, chances are 2 in 3 that it will return in future pregnancies. Many women who have gestational diabetes go on to develop type 2 diabetes years later. Certain basic lifestyle changes may help prevent diabetes after gestational diabetes; such as losing weight, making healthy food choices and exercising regularly.
* Dr Kumari Varghese MBBS, MD (Gynaecology), DGO is Specialist-Obstetrics & Gynaecology at Aster Medical Centre, Al Hilal
GULF TIMES
