First isolated in June 2012 in the city of Jeddah,
Mers has infected at least 77 people and killed at
least 40 of them. Now, the deadly virus has
prompted global battle plans. By Eryn Brown
|
|
In a war room of sorts in a neatly appointed government building, US officers dressed in crisp uniforms arranged themselves around a U-shaped table and kept their eyes trained on a giant screen. PowerPoint slides ticked through the latest movements of an enemy that recently emerged in Saudi Arabia — a mysterious virus that has killed more than half of the people known to have been infected.
Here at the Centers for Disease Control and Prevention, experts from the US Public Health Service and their civilian counterparts have been meeting twice a week since the beginning of June to keep tabs on the Middle East Respiratory Syndrome Coronavirus. Mers-CoV, as the pathogen is known, causes fevers, severe coughs and rapid renal failure as it attacks the lungs of victims.
Since it was first isolated in June 2012 in the city of Jeddah, Mers has infected at least 77 people and killed at least 40 of them. The number of confirmed cases has quadrupled since April, and patients have been sickened as far away as Tunisia and Britain. Most troubling to health experts are reports of illnesses in patients who have not been to the Middle East.
The virus has not yet emerged in the US, and perhaps it never will. But in July and August, towards the end of the holy month of Ramadan, around 11,000 American Muslims will travel to the Arabian Peninsula. In the meantime, millions more will fly between continents, citizens of today’s globalised world.
“A person from New York could go to Saudi Arabia for business and carry the virus home on the way back,” said Matthew Frieman, a virologist at the University of Maryland School of Medicine in Baltimore. “There’s zero reason why that couldn’t happen.”
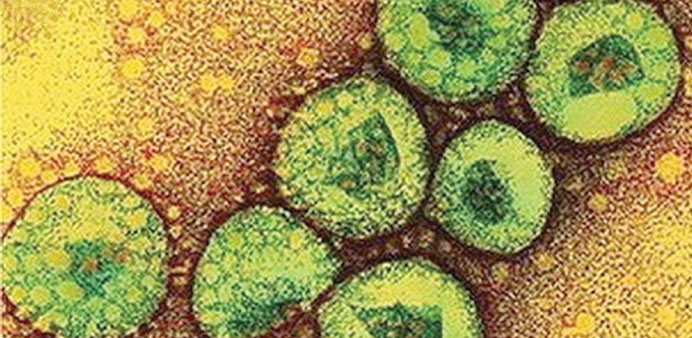
Many of the scientists working to understand Mers are veterans of the 2003 outbreak of severe acute respiratory syndrome, or Sars. A previously unknown coronavirus — a sphere-shaped virus spiked with proteins that make it look like it has a corona, or halo — jumped from its bat hosts and started infecting and killing people in China and Hong Kong.
By July 2003, more than 8,400 people around the world had become ill with Sars, which spread rapidly in hospitals. There were no fatalities in the US, but the World Health Organisation (WHO) warned travellers to avoid Toronto after 16 deaths there.
The epidemic was over within a year thanks to effective infection-control practices like wearing masks, identifying patients quickly and treating their symptoms promptly. By then, more than 800 people had died and local economies suffered $30bn in losses, according to WHO estimates.
Scientists hadn’t thought coronaviruses, known for causing colds and stomach woes, could be so dangerous. After Sars, they started taking the viruses seriously. So when a coronavirus killed the patient in Jeddah, researchers pounced. “We’ve always speculated that there could be another outbreak that could be as lethal as Sars,” Frieman said.
Teams around the world starting sequencing the virus’ genetic code. They determined that Mers must have emerged sometime in 2011.
Other researchers kept track of Mers victims. They reported sporadic cases in Saudi Arabia and Jordan, then in England, France and Italy, where patients had gone to seek medical treatment. Most of the victims were men, and many already had problems like heart disease and diabetes that may have contributed to their illnesses.
Epidemiologists started noticing clusters of Mers cases in families and in hospitals, in people who had close contact with victims. That made researchers worry that the virus might evolve to spread more easily from person to person — a prerequisite for a pandemic.
One such instance was described in May in the medical journal Lancet. It began in mid-April with a 64-year-old man who had diabetes and had received a kidney transplant in 1998.
Five days after travelling from Dubai to France, he developed a cough and breathing problems and was admitted to a hospital in Valenciennes, where he shared a room with a 51-year-old man being treated for a blood clot in a vein in his arm.
After three days, the older patient was transferred to an intensive care unit, where his respiratory symptoms worsened and his kidneys began to fail.
Doctors began to suspect Mers on May 1, and their suspicions were confirmed about a week later. The patient died of multiple organ failure.
Meanwhile, the younger man was discharged from the hospital on April 30 but started having respiratory troubles about a week later. He had a history of heart disease, and his bed had been five feet away from the patient with Mers. He was admitted to an intensive care unit, where tests revealed he was infected with the same virus. He developed a fever, and his lungs and kidneys began to fail. He spent several weeks in the intensive care unit and was still alive when the report was published in May 29.
By the end of May, health officials had identified a particularly large cluster of 26 people who fell ill in Saudi Arabia’s Al-Ahsa region, as well as smaller clusters in Britain, Italy and Tunisia.
That uptick may have reflected a surge in infections and deaths — or perhaps just health workers doing a better job of testing and reporting new cases, said Dr Ian Lipkin, an epidemiologist at Columbia University in New York.
“We don’t know: Is it new information, or is it information we should have had before?” he said.
There are many important details about Mers that scientists haven’t yet been able to figure out.
For instance, researchers think that Mers, like Sars, comes from bats — but they aren’t entirely certain. They also don’t know whether the virus spreads to pets or livestock before it strikes people or how it would do so, said Christian Drosten, head of the Institute of Virology at the University of Bonn Medical Center in Germany.
Scientists are still perfecting their methods to test for the virus in ailing patients. Swabs from nasal passages and throats don’t seem to pick up the pathogen as well as samples from deep in the lungs. Experts don’t know how many people may have been infected with Mers without getting sick from it, Drosten said.
Researchers also need a more complete understanding of the health problems the Mers victims had before they got sick, Frieman said, adding that the information would “crucially affect” the work in his lab.
Public health officials, meanwhile, are readying their response on the ground. The World Health Organisation is tracking the outbreak. In June, representatives from the United Nations agency travelled to Saudi Arabia to review the response to Mers, including stepped-up efforts to identify infected people and new measures to prevent infections in hospitals.
The CDC response team is working with other countries and with medical facilities in the US to make sure procedures are in place to combat Mers. Hospitals have received guidelines for assessing and isolating patients to keep the virus contained.
“If there are cases that come to the US, we want to be well-prepared to address them,” said CDC Director Dr Thomas Frieden.
During the briefing in the CDC boardroom, the response team briskly considered a variety of issues: Which states have labs to test for Mers? How were scientists the National Institutes of Health prioritising different types of Mers research? Would it be feasible to create a video about Mers to screen on flights arriving from overseas? Could social media help alert people to the potential danger?
Mers has been suspected in about 40 people in the US, but tests revealed that none had the virus. Even if that luck holds, experts insist that their efforts to understand Mers — and to bring the international community into the fold to combat it — are an investment in the future, when another mysterious pathogen starts sickening people.
“This is the type of emerging infection we will inevitably see more of,” Frieden said. — Los Angeles Times/MCT