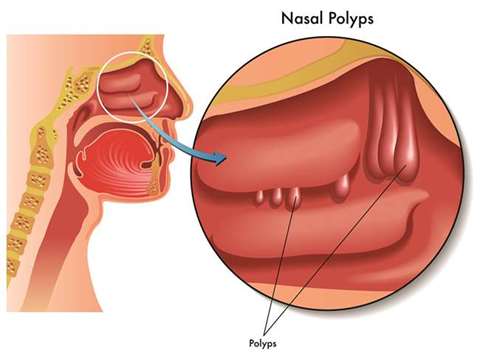
Nasal polyps are soft, painless, noncancerous growths on the lining of your nasal passages or sinuses. They hang down like teardrops or grapes. They result from chronic inflammation due to asthma, recurring infection, allergies, drug sensitivity or certain immune disorders. Small nasal polyps may not cause symptoms. Larger growths or groups of nasal polyps can block your nasal passages or lead to breathing problems, a lost sense of smell, and frequent infections.
Nasal polyps can affect anyone, but they’re more common in adults. Medications can often shrink or eliminate nasal polyps, but surgery is sometimes needed to remove them. Even after successful treatment, nasal polyps often return.
Symptoms
Nasal polyps are associated with inflammation of the lining of your nasal passages and sinuses that lasts more than 12 weeks. However, it’s possible and even somewhat more likely to have chronic sinusitis without nasal polyps.
Nasal polyps themselves are soft and lack sensation, so if they’re small you may not be aware you have them. Multiple growths or a large polyp may block your nasal passages and sinuses.
Common signs and symptoms of chronic sinusitis with nasal polyps include runny nose, persistent stuffiness, post nasal drip, decreased or absent sense of smell, loss of sense of taste, facial pain or headache, pain in your upper teeth, a sense of pressure over your forehead and face, snoring and itching around your eyes.
When to see a doctor
See your doctor if your symptoms last more than 10 days. Symptoms of chronic sinusitis and nasal polyps are similar to those of many other conditions, including the common cold.
Seek immediate medical care if you experience serious trouble in breathing, sudden worsening of your symptoms, double vision, reduced vision or limited ability to move your eyes, severe swelling around your eyes and increasingly severe headache accompanied by high fever or inability to tip your head forward.
Causes
It’s not clear why some people develop chronic inflammation or why ongoing inflammation triggers polyp formation in some people and not in others. The inflammation occurs in the fluid-producing lining (mucous membrane) of your nose and sinuses. There’s some evidence that people who develop polyps have a different immune system response and different chemical markers in their mucous membranes than do those who don’t develop polyps.
Nasal polyps can form at any age, but they’re most common in young and middle-aged adults. Nasal polyps may form anywhere in your sinuses or nasal passages, but they appear most often in an area where sinuses near your eyes, nose and cheekbones all drain through winding passages into your nose.
Risk factors
Any condition that triggers chronic inflammation in your nasal passages or sinuses, such as infections or allergies, may increase your risk of developing nasal polyps. Conditions often associated with nasal polyps include:
* Asthma, a disease that causes overall airway inflammation and constriction.
* An allergy-like response to aspirin or to pain relievers such as ibuprofen (Advil, Motrin, others) and naproxen (Aleve).
* Allergic fungal sinusitis, an allergy to airborne fungi.
* Cystic fibrosis, a genetic disorder that results in the production and secretion of abnormally thick, sticky fluids, including thick mucus from nasal and sinus membranes.
* Churg-Strauss syndrome, a rare disease that causes the inflammation of blood vessels.
Your family history also may play a role. There’s some evidence that certain genetic variations associated with immune system function make you more likely to develop nasal polyps.
Complications
Nasal polyps can cause complications because they block normal airflow and fluid drainage, and also because of the chronic inflammation underlying their development. Potential complications include:
* Obstructive sleep apnea. In this potentially serious condition, you stop and start breathing frequently during sleep.
* Asthma flare-ups – chronic rhino sinusitis can trigger asthma attacks.
* Sinus infections – nasal polyps can make you more susceptible to sinus infections that recur often or become chronic.
* Spread of infection to your eye socket – if an infection spreads to your eye socket, it can cause swelling or bulging of your eye, inability to move your eye, reduced vision or even blindness that can become permanent.
* Meningitis – infection can also spread to the membranes and fluid surrounding your brain and spinal cord.
* Aneurysms or blood clots – infection can cause problems in the veins surrounding the sinuses, interfering with the blood supply to parts of your brain and putting you at risk of a stroke.
Tests and diagnosis
The doctor can usually make a diagnosis based on your answers to questions about your symptoms, a general physical exam and an examination of your nose. Polyps may be visible with the aid of a simple lighted instrument.
Other diagnostic tests include:
* Nasal endoscopy – a nasal endoscope, a narrow, flexible tube with a lighted magnifying lens or tiny camera, enables your doctor to perform a detailed examination inside your nose and sinuses. He or she inserts the endoscope into a nostril and guides it into your nasal cavity.
* Imaging studies – images obtained with computerised tomography (CT) or magnetic resonance imaging (MRI) can help your doctor pinpoint the size and location of polyps in deeper areas of your sinuses and evaluate the extent of inflammation. These studies may also help your doctor rule out the presence of other possible obstructions in your nasal cavity, such as structural abnormalities or another type of cancerous or noncancerous growth.
* Allergy tests – your doctor may suggest skin tests to determine if allergies are contributing to chronic inflammation. With a skin prick test, tiny drops of allergy-causing agents (allergens) are pricked into the skin of your forearm or upper back. The drops are left on your skin for 15 minutes before your doctor or nurse observes your skin for signs of allergic reactions. If a skin test can’t be performed, your doctor may order a blood test that screens for specific antibodies to various allergens.
* Test for cystic fibrosis – if you have a young child diagnosed with nasal polyps, your doctor may suggest testing for cystic fibrosis, an inherited condition affecting the glands that produce mucus, tears, sweat, saliva and digestive juices. The standard diagnostic test for cystic fibrosis is a noninvasive sweat test, which determines whether your child’s perspiration is saltier than most people’s sweat.
Treatments Medications
Nasal polyp treatment usually starts with drugs, which can make even large polyps shrink or disappear. Drug treatments may include:
* Nasal corticosteroids
* Oral and injectable corticosteroids
* Other medications
Surgery
If drug treatment doesn’t shrink or eliminate nasal polyps, your doctor may recommend surgery. The type of surgery depends on the size, number and location of your polyps and the extent of inflammation. Surgery options for nasal polyps include:
* Polypectomy. Small or isolated polyps can often be completely removed using a small mechanical suction device or a microdebrider — an instrument that cuts and extracts soft tissue. This procedure, called a polypectomy, is performed on an outpatient basis.
* Endoscopic sinus surgery – you may need surgery to remove polyps and to correct problems with your sinuses that make them prone to inflammation and polyp development. The surgeon inserts an endoscope, a small tube with a magnifying lens or tiny camera, into your nostrils and guides it into your sinus cavities. He or she uses tiny instruments to remove polyps and other obstructions that block the flow of fluids from your sinuses. Your surgeon may also enlarge the openings leading from your sinuses to your nasal passages. Endoscopic surgery is usually performed as an outpatient procedure.
After surgery, you’ll likely use a corticosteroid nasal spray to help prevent the recurrence of nasal polyps. Your doctor may also recommend the use of a saltwater (saline) rinse to promote healing after surgery.
Prevention
You may help reduce your chances of developing nasal polyps or having nasal polyps recur after treatment with the following strategies:
* Manage allergies and asthma
* Avoid nasal irritants
* Practice good hygiene
* Humidify your home
* Use a nasal rinse or nasal lavage.
* Dr Agish Mathew Peter, MD, MS (ENT) is an ENT Surgeon at Aster Hospital, Doha
INDICATIONS: Small nasal polyps may not cause symptoms. Larger growths or groups of nasal polyps can block your nasal passages or lead to breathing problems, a lost sense of smell, and frequent infections.
