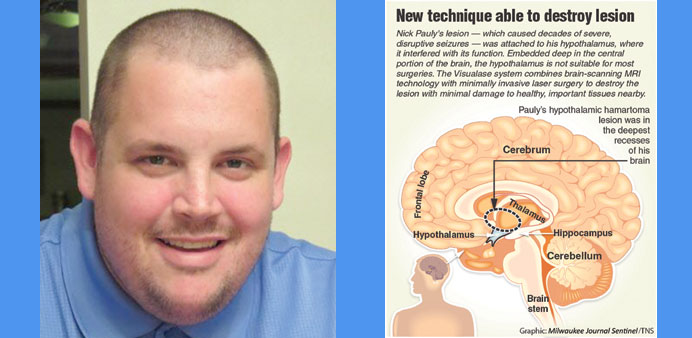
FINALLY: Nick Pauly went through two surgeries using the recently-developed Visualase system to treat a previously-inoperable hypothalamic lesion that caused disruptive seizures.
By Eric Hamilton
The seizures caused Nick Pauly to laugh mirthlessly, clap his hands and shout.
At times, he would swear loudly.
The seizures would come on without warning, caused by a tumour-like lesion that interfered with his hypothalamus — a crucial brain structure involved in sleep, learning and cognition.
Medication could not control the seizures, and for the vast majority of his 30 years, there was no safe way to treat the lesion embedded in his brain.
But last year, surgeons at Froedtert Hospital and Children’s Hospital of Wisconsin used new technology to deliver laser light directly into the lesion, destroying the problematic tissue without damaging the area around it.
After two surgeries and remarkably short hospital stays, Pauly’s most severe seizures have stopped. Now, he is adjusting to life without the seizures, though he still struggles with the effects of living with the lesion for three decades.
Pauly grew up in Port Washington, Wisconsin, as the middle child between his older sister and younger brother with his mother, Mary Jo, and father, James. As a toddler, he failed to meet some developmental milestones and would chuckle to himself, leading to a diagnosis of gelastic — or laughing — epilepsy. He was born with the lesion clinging to his hypothalamus, known as a hypothalamic hamartoma, which caused the disruptive seizures and led to developmental delays and permanent cognitive deficits.
The laughing seizures were nearly impossible to control.
Pauly has “been on almost every seizure medication there is,” said Mary Jo, who spends a great deal of time helping coordinate his medical care.
The seizures would surprise people nearby, and Pauly suffered from emotional outbursts and other behavioural problems linked to his lesion. His cognitive impairment is midrange; he reads at a fifth-grade level.
Despite these challenges, Pauly graduated from high school and had success in finding and landing jobs — although he had trouble keeping them. He lived independently. The Port Washington community supported him.
“He’s got a big heart, and he’s very kind,” said Mary Jo. “There’s a really wonderful side to him that most people see.”
But last year, Pauly’s seizures grew worse. They would last longer, sometimes as long as 30 seconds. They became louder and would happen frequently at night, disturbing his neighbours. His landlord did not renew his lease, and he had to move back home.
The worsening seizures ultimately led Pauly to Wade Mueller and Sean Lew, neurosurgeons at Froedtert and Children’s Hospital, respectively. In 2013, they had performed the hospitals’ first surgery using new technology, called Visualase, designed to treat previously inoperable lesions such as Pauly’s. Their team of epilepsy specialists agreed that Pauly was a good candidate for the surgery.
His surgery was scheduled for August 14, 2014.
Mueller and Lew have collaborated on each of the Visualase surgeries at the hospitals, along with a team that includes an anesthesiologist, a radiologist and a technician from Medtronic, the distributor of Visualase. The FDA approved the technology in 2007, and it has since been used in more than 1,000 surgeries.
The Visualase system combines a brain-scanning MRI with minimally invasive laser surgery. Surgeons insert a fibre, less than a tenth of an inch across, through a small hole in the skull, then through the upper layers of brain tissue and finally into the lesion, near the base of the brain. Infrared laser light travels down an optical fibre, where it is absorbed by the lesion and converted to heat. When the surrounding tissue gets hot enough, around 140 degrees or so, it is destroyed.
An MRI helps target the laser applicator, but just as important, it also monitors the temperature of the brain tissue. That allows surgeons to protect healthy tissue while delivering enough laser energy to damage the lesion.
“This little temperature thing is just golden,” said Mueller. “It’s what makes the thing so cool, and so safe.”
In all, the new technology adds $15,000 to each surgery, but it is covered by most insurance. Shorter hospital stays and better outcomes might make it cheaper than other surgeries in the long run. In Pauly’s case, it was the only treatment available.
Pauly was nervous going into his surgery in August, but he had his parents, aunts, sister and niece with him for support on that day.
The surgery had hiccups but was successful. After realising the laser applicator was off by a tenth of an inch, the surgical team had to restart the procedure to get the best positioning.
“It was in the lesion but it wasn’t perfect,” said Lew. “You need it to be perfect.”
The hamartoma was large, but after a surgery that lasted eight hours, most of the lesion was destroyed. Pauly’s seizures improved immediately.
“With Nick we got a very dramatic effect with his seizures. Like gone,” said Mueller.
As time went on, however, Pauly’s laughing seizures started to return, a sign that the remaining lesion tissue would need to be treated. He had one of the largest lesions treated at Froedtert and Children’s hospitals, and is the only patient who has required two surgeries of the nine treated at the hospitals since 2013.
About five months after his first surgery, Pauly went in for his second. The surgical team approached the hamartoma from the other side to target the areas they could not reach in the first surgery, and were able to destroy the rest of the lesion.
After the second surgery was over, Pauly felt relief.
“It was over. It was done,” he said in an interview. “I didn’t have to worry about it again.”
In the six months since then, the laughing seizures have not returned. It looks like he is in the clear.
Pauly lives in a group home he likes now, frequently taking trips to the museum or the movies with the woman who runs the home. He still has mild seizures, but most people would never notice, and they are much less frequent. You cannot tell where the laser applicator was inserted.
The imprint the lesion left on him remains, however. He has some hard-to-define memory problems that he calls “glitches,” and he still suffers from emotional outbursts.
“It’s a whole different ball game, and we’re not quite sure where we are in that,” said Mary Jo. “It’s too new.”
Although he gained weight by taking therapeutic steroids for the surgeries, and is still focused on recovering and adjusting to life after the procedure, Pauly is grateful to be free of the disruptive seizures that stuck with him for 30 years.
“It’s amazing what they can do now,” he said. — Milwaukee Journal Sentinel/TNS