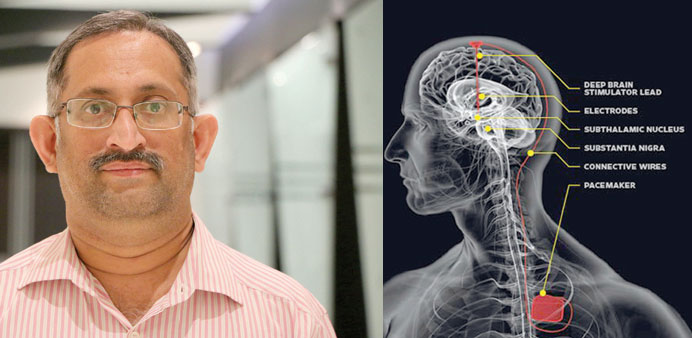
HELPING HAND: As soon as he gets the required support from hospitals here, Dr Ramnarayan hopes to treat Parkinson’s patients with DBS in Qatar as well. Photo by Umer Nangiana. Right: SOLUTION: This is how DBS works (for illustration purposes).
By Umer Nangiana
In the beginning, symptoms are as barely noticeable as a tremor in one hand. Gradually, it will change into major movement disorders causing tremors, stiffness and slowness of movement.
Parkinson’s disease is a progressive disorder of the nervous system that affects your movement. In the early stages, it shows little symptoms but the patient’s condition worsens as it progresses over time.
Although Parkinson’s disease has no cure, “medication and certain surgical procedures markedly improve symptoms, so much that in some cases they are not even noticed any longer.”
Dr R. Ramnarayan from India, a specialist in functional neurosurgery, who was in Qatar recently tells Community more about Parkinson’s disease and how he has successfully treated patients with Deep Brain Stimulation (DBS) technique in India and in other Gulf countries.
Trained in functional neurosurgery from UK, Dr Ramnarayan is a specialist in surgery for movement disorders, chronic pain epilepsy, spasticity, bowel or bladder dysfunction, patients in coma state and other such conditions.
From his periodic visits to Qatar, the specialist says he has found out that Parkinson’s disease is very common here, widespread as it is in the region starting from India up till Morocco in North Africa.
“The biggest problem with this disease is that it affects all movements. It causes three things; one is tremors, the shaking of the hands; the other is stiffness and rigidity so much of it that even smallest things become huge for patients and the biggest of them all is slowness of the movement,” says the neurosurgeon.
“Suppose, you tell me to go out of this room and let’s assume it will take me 3 to 4 seconds, but if I am suffering from this slowness of movement, it will take me 10 minutes or more,” he explains.
Dr Ramnarayan says the exact cause of the disease is not yet known. It is like diabetes in which the hormone called insulin becomes lesser and lesser. Similarly, there is a chemical called dopamine in the brain which has to work to enable us to make movements.
Due to some reasons which are not known yet, the dopamine level in the brain comes down and people with Parkinson’s disease become slow and stiff in their movements.
“It has no cure but with medical care and surgery, you can make them better,” says the medical expert, adding how he treats such patients referred to him.
“If you send a patient with Parkinson’s to me, what I will do first is take neurology opinion on whether this patient can do better with medicine, and there are good medicines. And most of the patients for a good number of years do well with the help of medicines,” says Dr. Ramnarayan.
However, over a period of time the patients come out of medicine as they start causing more side effects then effects.
Why does that happen?
The action of the medicine becomes less effective and thus the patient starts taking over-medication which results in increased side-effects. It is at this stage, says Dr Ramnarayan, you need to operate on the patient and results have shown that they do very well post-operation.
“In fact, I have had patients, who stopped medication completely and they are doing very well,” claims the neurosurgeon.
After doing certain assessments and determining that a patient is suffering from side-effects and the medicine is not doing any good to him, Dr Ramnarayan offers them surgery.
The surgery is called Deep Brain Stimulation (DBS). The neurosurgeon from India, who has successfully conducted on a number of patients from different countries explains what DBS is and how it is done.
Each part of the brain has got different functions. There is an area of the brain called ‘subthalamic nucleus,’ and when you stimulate that area, all the symptoms of the disease come down.
“It is situated very deep in the area. So what this surgery involves is putting two electrodes into this area connected with what we call brain pacemaker,” says the doctor.
They put a battery under the front of the chest of the patient and connect it to the electrodes that are put in the brain and it stimulates continuously. So each patient by trial and error would do so well that sometimes you would not recognise that this person had this problem previously, claims Dr Ramnarayan.
It is a continuous function and everything is inside the body and the patient does not see anything except for a small scar on his chest.
However, it is indeed a very complicated procedure as it involves connecting the electrodes in the brain with the battery placed under the chest. And this is the reason why it cannot be done at most places. It involves, and needs a lot of support from the system.
These are all pinhole surgeries, however, they do not require patients to stay in the hospital for a long time or remain in the intensive care. The patient can walk home the very next day the surgery is done.
“Suppose I have a patient admitted on Saturday, I operate on him on Sunday, usually the patient walks out on Monday. And there is no need to keep these patients in ICU or putting them on ventilators,” says Dr Ramnarayan.
Also, during the surgery, the patient remains conscious as it is done under the local anesthesia except for the last 15 minutes when the battery has to be placed under the chest.
“The reason you have to do it under local anesthesia is that you are putting electrodes into the brain through a pinhole so you need to know where you are going and the only way to do so is by doing what we call micro electrode recordings,” says the surgeon.
Before the surgery, he spends time with the patients, explains to them the procedure and makes them very comfortable because their cooperation is very essential. During the surgery, the patient is asked to make movements so that the surgeon knows, through the waves on the screen, where exactly is he or she going.
During the surgery, he has to keep monitoring the waves generated by the brain continuously and, in fact, does have a team of trained personnel who constantly monitor these waves and inform him about any changes in their movement immediately.
“That is why I am saying it requires a lot of support from the system and it is not just about finances. You need human resources’ support. You need people who are trained to do this,” says the surgeon.
In Qatar, he has not conducted any operations yet; however, he is trying to make some hospitals here arrange for the support system so that it can be done locally.
He has operated upon patients from Oman and Dubai (UAE) in the Gulf region and they are all doing well, he says. The surgeon says he selects his patients very carefully as he says this operation like any other operation is better done on people at an early stage of the disease.
As soon as he gets the required support from the hospitals here, Dr Ramnarayan hopes to treat Parkinson’s disease patients with DBS here in Qatar as well.