|
|
The cervix is part of a woman’s reproductive system. The cervix is the lower, narrow part of the uterus (womb).
Statistics
Cervical cancer is second most common cancer in women worldwide. In Qatar, cervical cancer incidence follows only to breast cancer. According to WHO report, every year more than 270,000 women die of cervical cancer. Cervical cancer used to be the leading cause of cancer death for women all over the world. However, in the past 40 years, the number of cases of cervical cancer and the number of deaths from cervical cancer have decreased significantly.
This decline largely is the result of many women getting regular Pap test, which can find cervical precancer before it turns into cancer.
The highest incidence of cervical cancer occurs in women aged between 30 and 39, with the under-35 most likely to be affected. The number of women affected by cervical cancer falls steadily after the age of 40, although there is a slight increase in women who are over 70.
In a general scenario, majority of women show awareness about Pap smear, but few of them actually go for cervical screening. That suggests some hindrance or fear or incomplete awareness about the test, which inspired me to write this article for community awareness.
Symptoms
Early cervical cancers usually don’t cause symptoms. When the cancer grows larger, women may notice abnormal vaginal bleeding:
Bleeding that occurs between regular menstrual periods/after sexual intercourse.
Menstrual periods that last longer and are heavier than before.
Bleeding after going through menopause.
Increased (foul smelling) vaginal discharge.
Pelvic pain/pain during sex.
Cervical cancer, infections, or other health problems may cause these symptoms. A woman with any of these symptoms should tell her doctor so that problems can be diagnosed and treated as early as possible.
Risk factors
The following risk factors increase the risk of cervical cancer:
l The most common cause is infection of the cervix with human papillomavirus (HPV).
Others
l Smoking.
l High number of full-term pregnancies.
l Long-term use of oral contraceptives.
What is Pap smear?
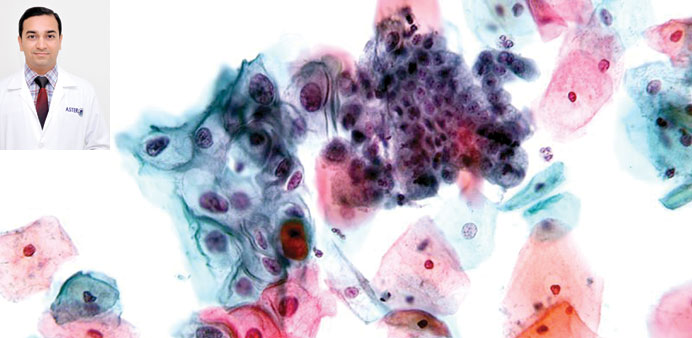
The cervical screening test, which is also called Pap (Papanicolaou) smear or test, is a major breakthrough for early detection of cervical cancer. It indicates general health of cervix, especially for cancer.
In 1928, after spending months observing his own wife’s cervical cells under a microscope, Dr George Papanicolaou invented the cervical smear as a method to detect cervical cancer. Dr Papianicolaou was given tribute by calling cervical smear as Pap smear and his discovery has indeed stood the test of time.
It is a well known fact that cervical cancer is getting less common cause of death, especially in countries where Pap smear screening is a routine protocol.
Procedure
In a Pap test (see diagram), the doctor uses a vaginal speculum to hold vaginal walls apart. Next, a sample of cells from the cervix is collected using a small cone-shaped brush and a tiny wooden spatula (1 and 2). The doctor then rinses the brush and spatula in a liquid-filled vial (3) or directly spreads over the slides and sends the sample to a laboratory for testing. It is essentially a painless procedure.
Benefit of Pap smear
Detecting cervical cancer early with a Pap smear gives you a greater chance at a cure. A Pap smear can also detect changes in your cervical cells that suggest cancer may develop in the future. Detecting these abnormal cells early with a Pap smear is your first step in halting the possible development of cervical cancer. On the other hand, Pap smear can avoid overaggressive treatment for certain lesions those may regress with time or medicines.
Who should have a Pap smear?
In general, doctors recommend beginning Pap smear testing at age 21 and then every two or three years. After age 30, Pap smears are generally recommended every three years, or every five years when the Pap smear is combined with an HPV test.
Pap smear may not be advised for:
l Women over 65 years of age.
l Women who had uterus and cervix removed (total hysterectomy).
l Sexually inactive women.
To ensure that your Pap smear is most effective, follow these tips prior to your test:
l Avoid intercourse, douching or using any vaginal medicines or spermicidal creams for two days before having a Pap smear, as these may wash away or obscure abnormal cells.
l Try not to schedule a Pap smear during your menstrual period.
The report may state one of the following:
l Inadequate smear.
l Normal: no further action required.
l Borderline: Suggest non-cancerous abnormality and may get back to normal after treatment. A follow up and repeat smear after 3-6 months is usually advised.
l Abnormal: in form of atypical cells or Intraepithelial lesion of low or high grade (LSIL or HSIL) or severe cell changes suggesting cancer.
Presence of abnormal cells does not always mean that you have cancer or will get cancer. It just means that some of your cells are abnormal and if they are not treated they may develop into cervical cancer. Many abnormal cells may go back to normal on their own.
Depending on the lesion, a colposcopy may be advised with requirement of biopsy, if indicated.
Abnormal changes in the cells of the cervix can be caused by certain types of the human papilloma virus (HPV). For most people, the virus goes away without treatment and does not cause any harm. There are high-risk and low-risk types of HPV. Types HPV-16 and HPV-18 are considered high risk for cervical cancer. If one is infected with these high-risk types of HPV, that person is more at risk of developing cancerous cells in cervix.
Test reliability
As with all screening tests, cervical screening is not 100% accurate. But regular screening can stop up to 75% of cancers from developing, but it does not prevent every case.
In recent years, many centres’ use Liquid-based cytology (LBC), this helps reducing artifacts in smears.
Prevention
A comprehensive approach towards cancer of cervix can prevent many cases, the approach should consist of: community education, regular screening, HPV vaccination and appropriate early treatment.
Avoiding certain risk factors and increasing protective factors may help prevent cancer.
Avoiding unsafe sexual activity by use of barrier contraceptives. Overall healthy habits (eg: healthy food, quitting smoking, regular exercise).
Getting an HPV Vaccine
Two HPV vaccines have been approved by the US Food and Drug Administration (FDA). The HPV vaccines have been shown to prevent infection with the two types of HPV that cause most cervical cancers. The vaccines protect against infection with these types of HPV for 6 to 8 years. It is not known if the protection lasts longer.
The vaccines do not protect women who are already infected with HPV. It can be given to females from 9 years of age till 25 years. Few studies suggest that vaccine given even after 25years of age, does offer some protection against HPV infection. It is important to note that even women who are vaccinated against HPV need to have regular Pap tests to screen for cervical cancer.
The Cervarix vaccine is produced by GlaxoSmithKline (GSK). It is called a bivalent vaccine because it targets two HPV types: 16 and 18.
The Gardasil vaccine is produced by Merck & Co, Inc. It is called a quadrivalent vaccine because it protects against four HPV types: 6, 11, 16, and 18. Gardasil is given through a series of three injections into muscle tissue over a 6-month period.
Regular Pap smear screening as advised by gynecologist.
WHO states that vaccination against HPV in girls nine to 13 years old combined with regular screening in women over age 30 for precancerous lesions followed by adequate treatment are key tools to prevent the 530,000 new cervical cancer cases diagnosed every year.
Further information can be obtained at:
l http://www.cdc.gov/cancer/cervical/index.htm
l http://www.who.int/reproductivehealth/topics/cancers/en/
l http://www.mayoclinic.com/health/pap-smear/MY00090
l Dr Chirag Sumanthlal Parmar is a pathologist at Aster Medical Centre in Al Hilal. Send your queries to [email protected]